While the news of the first CAR T-cell therapies approved by the U.S. Food and Drug Administration (FDA) was extraordinary, there were limits on eligibility. The FDA’s approval of Kite’s Yescarta® for diffuse large B-cell lymphoma in 2017 was for patients who had failed two or more lines of treatment.
Last week, the FDA increased the potential CAR T-cell patient pool by thousands.
The agency approved Yescarta for use after just one round of failed treatment, a move that expands who is eligible for the cancer cell and gene therapy. Additionally, patients will gain access to the therapy earlier in their treatment journey. They now have an alternative to undergoing a stem-cell transplant, which was the standard of care after an initial line of chemotherapy or immunotherapy failed.
Diffuse large B-cell lymphoma is the most common type of non-Hodgkin lymphoma, diagnosed in around 18,000 people in the U.S. each year. According to the American Journal of Managed Care, this FDA approval will grant access to CAR T cells for approximately 11,000 additional lymphoma patients.
Yescarta approved for use before stem-cell transplant

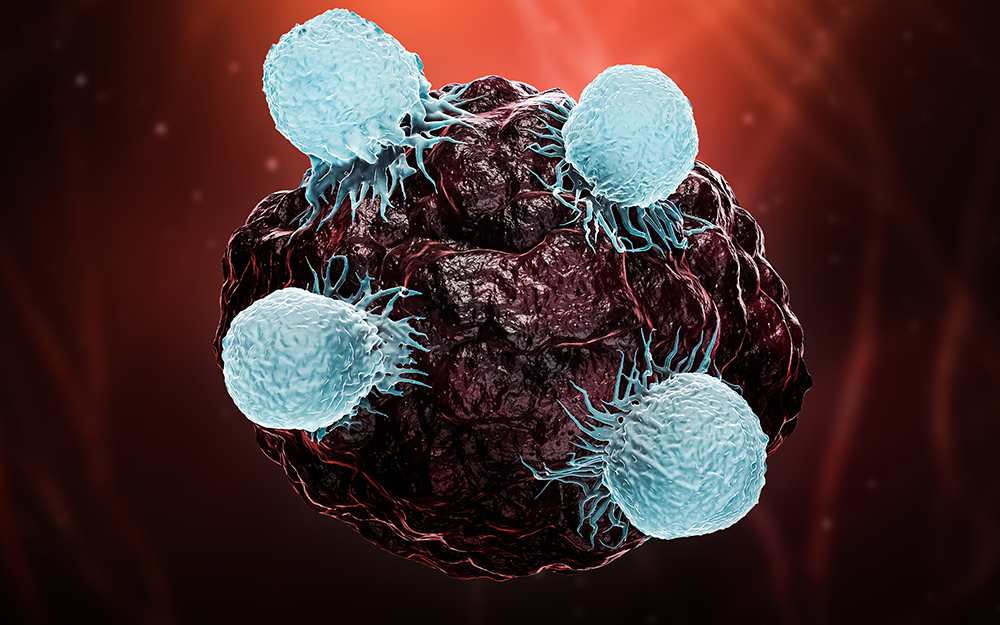
CAR T-cell therapy is a combination of cell therapy and gene therapy that boosts the power of the immune system. CAR is the acronym for chimeric antigen receptor.
Doctors remove patients’ T cells, which are usually incapable of fighting lymphoma tumors naturally. They send the T cells to a laboratory, where scientists add gene-specific protein receptors capable of targeting the lymphoma cells. The empowered T cells are returned to the hospital and infused back into the patient, who now has stronger versions of T cells, called CAR T cells, to fight their cancer.
Yescarta is an anti-CD19 CAR T-cell therapy, meaning it targets the CD19 protein expressed on cancerous B cells. Scientists add an antigen receptor genetically manufactured to target cells with the CD19 protein.
The initial line of therapy for this type of lymphoma is chemotherapy or immunotherapy. This is called the “standard of care.” Prior to this most recent FDA approval, the standard-of-care second line of therapy was chemotherapy plus a stem-cell transplant. Both lines of therapy needed to fail at controlling the lymphoma tumor before Yescarta CAR T-cell therapy became an option.
Yescarta is now approved for diffuse large B-cell lymphoma cases meeting one of two descriptions:
- Lymphoma tumors resistant to first-line chemotherapy – meaning the tumor never responds to the treatment
- Tumors that responded positively (shrank) due to chemotherapy but started re-growing (relapsed) within 12 months of chemotherapy ending
ZUMA-7 clinical trial leads to approval
The results of the ZUMA-7 clinical trial spearheaded the new FDA approval. The study included 359 patients and 77 cancer institutions.
Patients were slotted into either the Yescarta CAR T-cell arm or the standard-of-care (stem-cell transplant) arm. Two-thirds of the study participants were in the Yescarta arm and one-third were designated for stem-cell transplant.
Alliance for Cancer Gene Therapy reported on the trial’s success at the end of 2021. The phase 3 trial results were presented by Gilead at the American Society of Hematology annual meeting. Yescarta outperformed standard of care (stem-cell transplant with chemotherapy) in every survival-based statistical measurement:
- Yescarta reached a 61% two-year survival rate, better than standard of care’s 52% rate.
- Yescarta accomplished a 40.5% two-year progression-free survival rate (no new signs of tumor spread) versus 16% for standard of care.
- Yescarta had an 83% overall response rate (tumors either stalling in growth or shrinking) compared to 50% rate for standard of care.
- Yescarta posted a 65% complete response rate (no signs of tumors on scans) versus 32% for standard of care.
““Definitive clinical trial results such as these do not come along often and should drive a paradigm shift in how patients with relapsed or refractory (large B-cell lymphoma) are treated moving forward. Patients who do not respond to or relapse after initial treatment should quickly be referred to a CAR T-cell therapy authorized treatment center for evaluation.”” — Jason Westin, MD, the principal investigator for the ZUMA-7 clinical trial and an associate professor in the Department of Lymphoma and Myeloma at the University of Texas MD Anderson Cancer Center
Additionally, patients were far more likely to begin CAR T-cell therapy compared to stem-cell transplant. Nearly three times as many patients in the Yescarta arm of the clinical trial compared to the stem-cell transplant arm received their designated therapy.
““What we found was that (Yescarta) resulted in three times as many patients receiving treatment with curative intent, and an overall better outcome for patients than the previous standard of care. Additionally, we have now amassed significant experience with CAR T-cell therapy to better manage or prevent side effects, making this treatment more accessible for older patients and those with medical conditions for whom the standard of care might be difficult.”” — Frederick Locke, MD, ZUMA-7 lead investigator and co-head of the Immuno-Oncology Program at Moffitt Cancer Center
Between 30% and 40% will need second-line treatment due to their tumor not responding to chemotherapy or relapsing quickly after therapy ends.
Alliance for Cancer Gene Therapy promoting CAR T-cell therapies
Alliance for Cancer Gene Therapy previously published an article about this expected approvallisocabtagene maraleucel, or liso-cel). The Alliance reported the FDA is planning to rule on this treatment’s application as a second-line option in June.

Yescarta’s initial approval for diffuse large B-cell lymphoma is tied to Alliance for Cancer Gene Therapy’s early work to fund CAR T-cell therapy research projects. One of those projects was spearheaded by Carl June, MD, of Penn Medicine’s Abramson Cancer Center. Dr. June’s work led to the development of the first live-saving CAR T-cell therapies for specific types of leukemia and lymphoma, including large B-cell lymphoma.
Alliance for Cancer Gene Therapy will continue to promote the use of CAR T-cell therapy for not only blood cancers like lymphoma but also solid tumor diseases. The Alliance funds research projects at top cancer centers in the hopes of providing patients with more treatment options than just chemotherapy or radiation.
The FDA’s approval of Yescarta as a second-line therapy for diffuse large B-cell lymphoma is further proof that CAR T cells can defeat tumors. If you have donated to Alliance for Cancer Gene Therapy in the past, please continue to support our mission with a generous donation. If you are a potential first-time donor, let us explain why our non-profit organization is a needed entity in the effort to find cures for cancer.
Page sources
- Yescarta® Receives U.S. FDA Approval as First CAR T-cell Therapy for Initial Treatment of Relapsed or Refractory Large B-cell Lymphoma (LBCL). Gilead. Retrieved from: https://www.gilead.com/news-and-press/press-room/press-releases/2022/4/yescarta-receives-us-fda-approval-as-first-car-tcell-therapy-for-initial-treatment-of-relapsed-or-refractory-large-bcell-lymphoma-lbcl. Accessed: 04/03/2022.
- Diffuse Large B-Cell Lymphoma. Lymphoma Research Foundation. Retrieved from: https://lymphoma.org/aboutlymphoma/nhl/dlbcl/. Accessed: 04/03/2022.
- With Approval for Axi-cel in Second-line on the Horizon, CAR T-Cell Therapy Poised to Enter New Phase. American Journal of Managed Care. Retrieved from: https://www.ajmc.com/view/with-approval-for-axi-cel-in-second-line-on-the-horizon-car-t-cell-therapy-poised-to-enter-new-phase. Accessed: 02/16/2022.